How it works:
Step 1 uses My Way Cards, an online, illustrated patient-decision aid, to generate your Natural Dying Living Will[1]. Each of the 50 cards illustrates and describes one end-of-life or advanced-dementia condition written at the third-grade level of comprehension. Together, these conditions strive to comprehensively reflect what people dread most about being forced to endure prolonged dying in advanced dementia and other terminal illnesses. The descriptions are behavioral, not diagnostic. For example, if you cannot move your body irreversibly, even to say hello, how much difference does it make if you are living in an advanced stage of dementia, a persistent vegetative state, had a stroke, or living with ALS (Lou Gehrig’s disease)? Using behavioral criteria reduces potential conflict over the correct diagnosis and reflects what people care about most: losses of functioning and unwanted, embarrassing behaviors. The most important questions are not about diagnosis, but rather: Is your condition irreversible? and, Will it cause you and/or your loved ones to experience severe suffering?
You can complete the My Way Cards program using your computer, tablet, or cellphone. (A printed version is available upon request.) For each condition, you will be asked to respond to:
Based on your lifelong values and treatment preferences, do you judge this condition will, by itself, cause severe enough suffering to want to be allowed to die of your underlying disease?
If your answer is, “No or mild suffering that is not enough,” then you may decide you want to receive cardiopulmonary resuscitation (CPR) with Full Treatment, or DNR but Full Treatment otherwise. But if you depend on a caregiver to feed and hydrate you, and you still enjoy life, you can choose a POLST that orders CPRL. This means only one Full CPR attempt, and then—if successful—
Selective/Limited Treatment, so you will not be subjected to burdensome, invasive treatment including CPR. Your code status will be DNR.
If you judge your suffering will be severe from a condition, you can express your wish that your physician implement orders for Natural Dying (ND), which can be clinically effective to allow you to have a timely dying—even if you have “No Plug to Pull,” which means sustaining your life does not depend on receiving high-tech medical treatment. In contrast to some living wills, the Natural Dying living will does not demand withholding of food and fluid, which can be criticized as euthanasia. Instead, it withdraws assistance with assisted oral feeding and hydrating by caregivers’ hands. The two orders for Natural Dying are:
“Cease assisted oral feeding” and “Always place food and fluid within the patient’s reach.”
Note: Other living wills can be completed in less time, but if they are not both effective and acceptable, they may not fulfill their purpose. Those in authority must accept the order when the time comes to implement your wishes, and many will insist on being able to view it as moral.[4]
Using the criterion, “how much suffering would the condition cause?” is more compelling and specific than criteria included in most traditional and the new crop of “dementia directives.”[3] For example, the question of, “Will the harms and burdens of treatment outweigh its benefits?” is a laudable goal in theory, but in practice is usually too vague. Judging that your “Quality of Life” is too low, or that your “indignity” is too high, are also vague. Worse, such questions could lead to judging the lives of others are not worth living, which could start a dangerous slippery slope.
Other living wills pinpoint a substage of the Functional Assessment Staging Tool (FAST scale), but this approach to timing has an underappreciated problem: FAST is a research tool; it was not designed for making end-of-life treatment decisions. More generally, a living will whose criteria are based on reaching clinical conditions may be flawed and lead to premature dying. Example: it would be premature to allow you to die once you no longer can recognize your close family members,” since you and they may still enjoy spending time with each other.[2] A 2022 critical review of a new crop of dementia-specific directives revealed all had one or more flaws that may lead to premature or prolonged dying.[3]
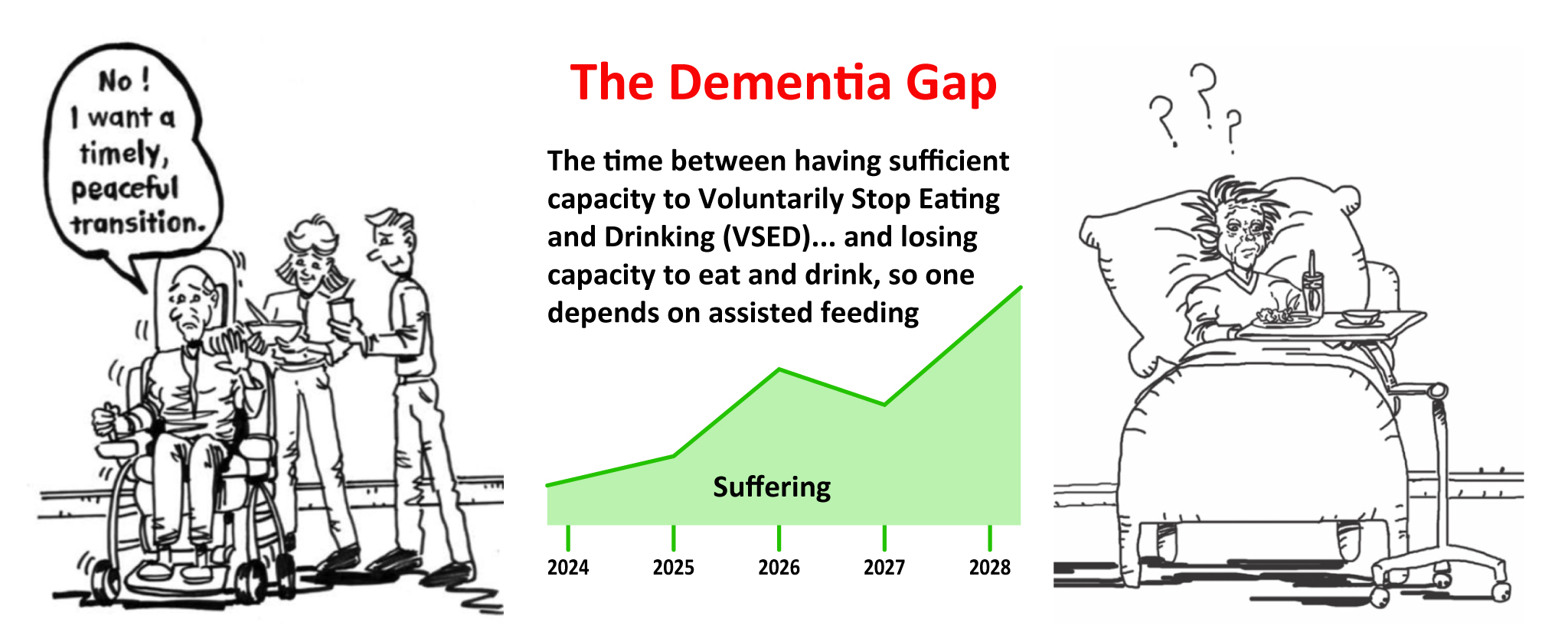
Until recently, another great challenge was unappreciated, yet for these unfortunate patients, all previously drafted living wills for dementia will not be able to fulfill their promise of delivering a peaceful and timely dying. I refer to their state as living in the Dementia Gap, which is illustrated and defined below. Patients living in the Dementia Gap have this “problem”: they can still eat and drink independently, so they cannot rely on their advance decision to refuse assisted oral feeding and hydrating (Natural Dying). Responding to this unique patient need, another intervention was developed in 2024. [Terman, S. A. (2024). Timely dying in dementia: To overcome the Dementia Gap, can Moderate Anesthesia be viewed as moral? (Manuscript in preparation.)
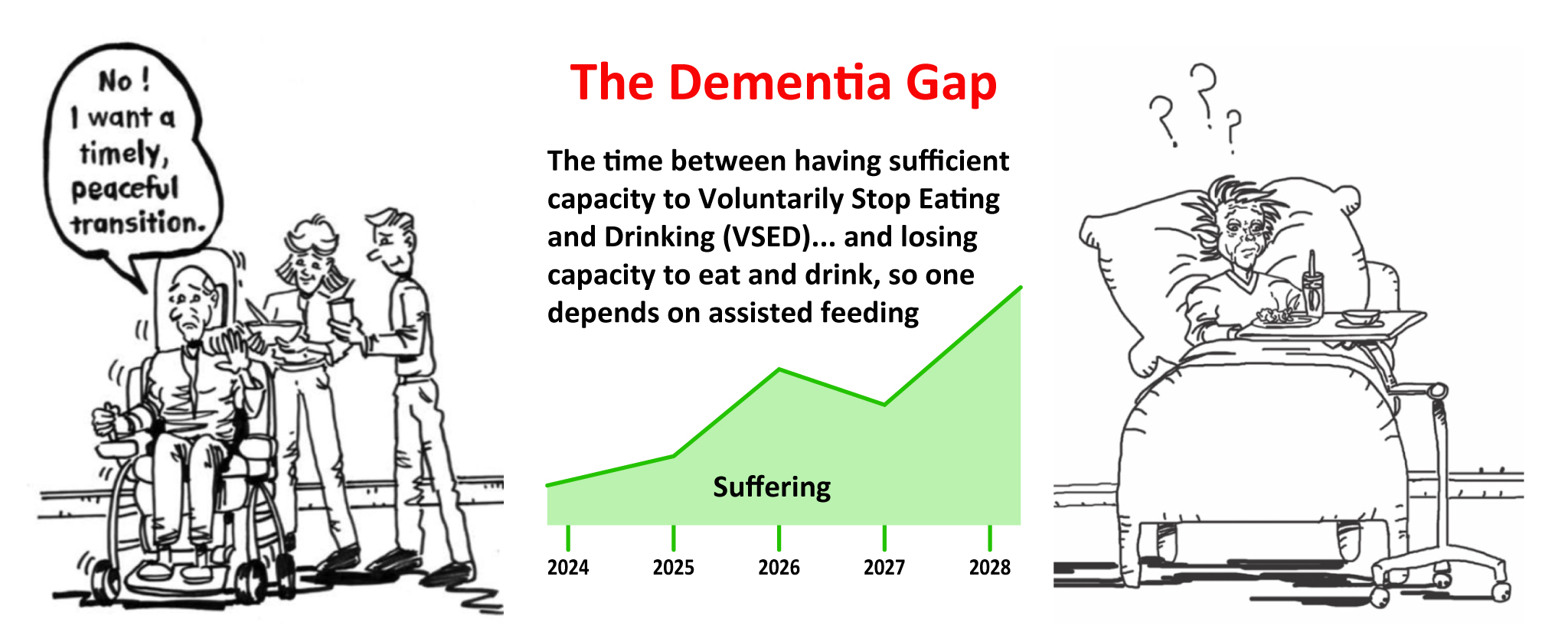
The Dementia Gap is a period of time. It begins with patients’ loss of capacity to exercise their right to refuse all food and fluid; that is, to Voluntarily Stop Eating and Drinking. The Dementia Gap ends when, due to the progression of dementia, patients lose their ability to eat and drink and need assistance from caregivers. Then then qualify for Natural Dying. Little is known about the Dementia Gap, such as its prevalence, and average and range of duration. So, no guideline is available to help physicians estimate how long their patients may remain in this state. Experience has shown, however, that loved ones of patients living in the Dementia Gap need proactive grief counseling.
You can choose to receive Moderate Anesthesia (MA) in advance, if you are in the Dementia Gap and reached two or more conditions you judged would cause exceedingly severe suffering. The level of sedation in MA is similar to that induced during endoscopy: a very deep sleep, so you do not respond purposefully to moderately loud verbal commands or to moderate tactile stimulation, but you do withdraw from painful stimuli, and you can breathe on your own without a respirator.
The new, purely clinical term, Moderate Anesthesia, is preferred to older terms such as palliative sedation to unconsciousness, or terminal sedation, since it does not imply a physician intent that opens the door for moral criticism. Yet MA can still be viewed as an “intervention of last resort” since there may be no other way to reduce the suffering of patients living in the Dementia Gap.
We still need to learn what the average and range of how long the Dementia Gap can last, what factors can help physicians estimate how long their patients may live in this state, and how many people are currently living in this state. (My forthcoming article estimates a million people.)
Your physician’s intent in inducing MA can be either to reduce the source of your suffering, or to decrease your awareness of suffering. The first has a foreseen, possible, but unintended side-effect of rendering you unconscious, and possibly ending your life earlier. The Rule of Double Effect may morally justify MA if your physician intended only the “good” effect (to reduce your suffering), but did not intend to use the possible “bad” effect (causing you to die) as the means to reduce your suffering.
Physicians may also intend to deliberately reduce your consciousness by slowly increasing the dose of sedating medications until you are no longer aware of your suffering.
To help prove your physician’s intent is to reduce your experience of suffering but not cause your earlier death, the “Respite Sedation” protocol can be used. You can agree to be awakened after about four days by reducing or stopping medications so your physician can ask you, “Has this rest allowed you to regain enough strength, so you want to continue to live and be awake?” (The part of the protocol cannot apply to PLADs since they will have lacked DMC before sedation and will therefore not be able to answer this question.)
Benefits of the patient decision aid, My Way Cards
Educates you about what it can be like, for you and your loved ones, to live with advanced dementia and other terminal illnesses with both illustrated cards and online videos.
Facilitates your making a clear and specific advance treatment decision for each condition, so you can express what intervention you want and when, based on your lifelong values.
Memorializes your wishes to inform your future physicians and others.
Reduces your agent’s emotional burden since they will be following your decisions, not making life-or-death decisions on your behalf. Your agent’s main role is to serve as your advocate by persuading your future treating physician and others to honor the treatment decisions that you previously made. Agents will only be asked to exercise their “substituted judgment” (their traditional role) if your living will does not include the condition you reached. Then, your agents will take into consideration your current condition and your future prognosis, and based on knowing your lifelong values and general treatment preferences well, strive to make the same decision you would have made.
Why this Step is Unique
The online program that uses My Way Cards to generate your Natural Dying Living Will strives to be comprehensive by including about fifty conditions. It can be your only living will since it is not merely an addendum. Since the descriptions of the conditions are illustrated and written at the thirdgrade level of reading comprehension, even early-stage dementia patients who experienced a decrease in cognitive functioning may be able to use it to express their end-of-life wishes.
Definition of the broadened concept of suffering
The online program that uses My Way Cards to generate your Natural Dying Living Will strives to be comprehensive by including about fifty conditions. It can be your only living will since it is not merely an addendum. Since the descriptions of the conditions are illustrated and written at the thirdgrade level of reading comprehension, even early-stage dementia patients who experienced a decrease in cognitive functioning may be able to use it to express their end-of-life wishes.
The broadened concept of suffering includes sources that cannot be detected by observing the patient.[2] They include: 1) physical pain that physicians and others may not detect; 2) emotional or psychic suffering; 3) existential suffering such as loss of meaning in life, fear of dying, and nearly total social isolation due to losing the ability to communicate due to inability to recognize loved ones and to recall significant life events; 4) disruption of life narrative, such as prior roles in one’s family, career, aand society that gave life meaning; 5) not being able to spare loved ones from emotional, physical, and financial suffering; 6) causing others to suffer by their empathy for your suffering; and 7) the dread of leaving tarnished memories with your future survivors. While such sources of suffering are not currently observable, many people, including physicians and providers, do not appreciate this point.[2]
The Natural Dying Living Will provides a way for your future physicians to answer the “when” question. Uniquely, they do not need to assess your contemporaneous suffering. Instead, physicians only need to answer this question, to determine if it is time for implementation:
Have you, my patient, reached a condition that you previously judged would cause you severe-enough suffering to want to be allowed to die from your underlying disease?