Why: Imagine receiving well-meaning but unwanted treatment that maintains your existence in an advanced stage of dementia—while you cannot articulate that your suffering is so severe, so difficult to detect, and so challenging to treat—that you prefer to be allowed to die. Further imagine that you currently do not know how, or are incapable of expressing your wish, to end your torment. Or, if you would consider stopping your intake of food and fluid, or receiving enough sedation to end your suffering, you would not know how to convince your future physicians/providers to comply with your wishes if they considered these treatments controversial based on their possibly hastening your dying.
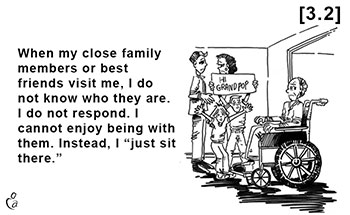
Dedicated healthcare providers may not be able to observe some sources of your suffering because your pain is not detectable, your disease is causing your loved ones to suffer, and/or your suffering will occur in your future. One example is leaving your survivors tarnished memories of yourself. Those who observe you in an advanced stage of dementia may conclude, “You are just sitting there,” but your existential suffering from losing important relationships has left you socially isolated and terribly lonely—after dementia has destroyed your sense of your own identity, your ability to recognize and communicate with others, and made you incapable of recalling past shared experiences.
The number of persons now living in advanced dementia (PLADs) is likely over two million in the U.S., and will likely double by 2050. While no one knows the precise percentage of patients whose suffering is severe, estimates are arguably between 25% to 50%. Caring for these patients can be physically, emotionally, and financially burdensome to patients’ family, friends, and society. The cost of care can climb to $125,000 annually. Some patients may live a decade. For those over 65, the risk of getting dementia doubles every five years; almost 10% have dementia; and one-third will die with dementia.
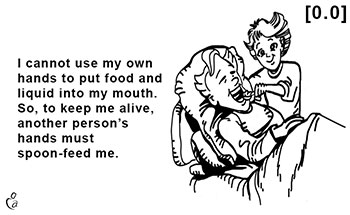
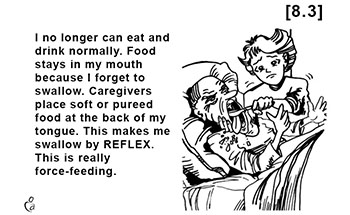
While assessing the intensity of your current suffering is elusive since many sources are non-observable, you can take effective action by planning ahead; that is, by completing Strategic Advance Care Planning. This protocol begins by asking you to judge 50 specific clinical conditions that you might someday reach. Your judgments for each condition’s potential to cause future suffering can then be based on your lifelong values and treatment preferences.
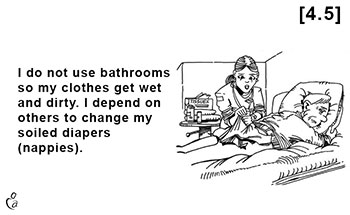
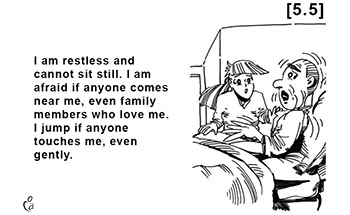
When: You must complete Strategic Advance Care Planning (Strategic ACP, SACP) while you still have decision-making capacity (DMC). DMC is the mental ability to perform the specific task of making conditional advance treatment decisions. “Conditional” means you have reached an observable future clinical “qualifying” condition. The premise that underlies this approach is that clinical conditions can be observed, but how much suffering they may cause is up to you to judge. DMC requires your ability to understand the treatment options, appreciate each option’s likely consequences, use rational thinking to render a diligent, deliberative decision, and to express this decision consistently over time. One advantage of Caring Advocates’ “My Way Cards” online program that generates your “Natural Dying Living Will” is that each of its 50 conditions is illustrated and written at the third-grade level of reading ability. Lowering the comprehensive level to complete this task makes it possible for many patients in early dementia to have sufficient DMC to complete their Natural Dying Living Will. Note: you can lose your DMC in ways other than dementia such as head trauma due to a car accident, a stroke, end-stage kidney or liver disease, other neurodegenerative diseases, and side-effects from medications, including pain relieving medications. You must complete DMC before any of these occur, so don’t delay in completing Strategic Advance Care Planning.
Who: Caring Advocates is a not-for-profit organization founded by, and continuously led by bioethicist/psychiatrist Stanley A. Terman, Ph.D., M.D., since 2000. The protocol, Strategic Advance Care Planning, is designed for people who want to control how and when they die (as much as feasible). Unlike other protocols, SACP does not stop after helping patients complete a comprehensive, clear and convincing, living will that states what treatments patients want if they reach a specific condition. (Note: “clear and convincing” is the highest standard of evidence in civil legal matters.) SACP adds layers of strategies to make success likely, where success is defined as patients receive the treatment they want. The Caring Advocates team can work with hospice if its medical and administrative leaders agree with the treatment that your Natural Dying Living Will instructed, although some authorities consider Natural Dying and Moderate Anesthesia controversial. If so, Caring Advocates may still be able to help without hospice. It depends on the specific circumstances that can be discussed.
How: Strategic Advance Care Planning has two parts: Planning and Implementation. You can create a plan now that is designed to be straightforward to implement later—even if Dr. Terman is not available. To explain: You can have a POLST Conversation with Dr. Terman, who will determine that you have DMC and share an adequate amount of information with you. Then, you can give your informed consent by signing/completing each POLST that contains medical orders written by Dr. Terman to fulfill your end-of-life goals. Example: you want to avoid a prolonged dying with suffering, and you want to live as long as you can still enjoy life, so you do not want your dying to be premature.
Each POLST is a set of specific immediately actionable physician orders that other health care providers are required to honor in all settings—including your home, hospital, skilled nursing facility, or luxury hotel to which you may move if comfort care cannot be obtained in your current residential setting. There are two exceptions to requiring other healthcare providers to honor your POLSTs, but they are infrequent. Both can be worked around. (A) Providers and institutions are required to reveal if they have a moral conflict with any intervention so that proxies/agents can seek treatment from other health care providers and institutions to provide the care that you desire. (B) Providers who claim the intervention requested is not consistent with generally accepted medical care must do so in good faith. Your proxy/agent may petition a court of law to prove this, and if they fail, they risk losing their legal immunity. Most importantly, your POLST and your Natural Dying Living Will can work together if you follow the recommendation of adding this order to each POLST: “POLST orders must be consistent with the patient’s directive (living will).”
Completing POLSTs requires four tasks. Dr. Terman and his staff routinely complete the first three:
- Dr. Terman or his staff can facilitate your deciding and memorializing which category of treatment you want upon reaching specific future clinical (qualifying) conditions. This task uses the online program of My Way Cards to generate a Natural Dying Living Will.
- Dr. Terman can, during the POLST Conversation, provide adequate information and determine if you have sufficient decision-making capacity to sign POLSTs whose orders could be life-determining.
-
Dr. Terman can write orders on POLST forms, so you can receive goal-concordant care.
Note that tasks 1 to 3 can be completed during advance care planning.
- If someday, you reach a “qualifying condition,” any physician/provider can implement the orders on these POLSTs, as explained below.
To explain: The usual and customary practice of medicine includes asking a currently treating physician to rely on the assessment and to carry out the orders that a previous physician wrote—if the patient’s clinical condition warrants these orders. While the needed orders may be legal, clinically appropriate, and moral, some physicians will still consider them controversial. If the currently treating physician refuses to implement a POLST, the proxy/agent must search for another physician who is willing. Since sabotage is possible after these orders are written, SACP also includes additional strategies designed to overcome them. An example: after you become an incapacitated person currently living with advanced dementia you may still request assisted feeding and hydrating even though you have reached a qualifying condition as expressed stated in your Natural Dying Living Will.